Laparoscopic Sleeve Gastrectomy
Sleeve Gastrectomy

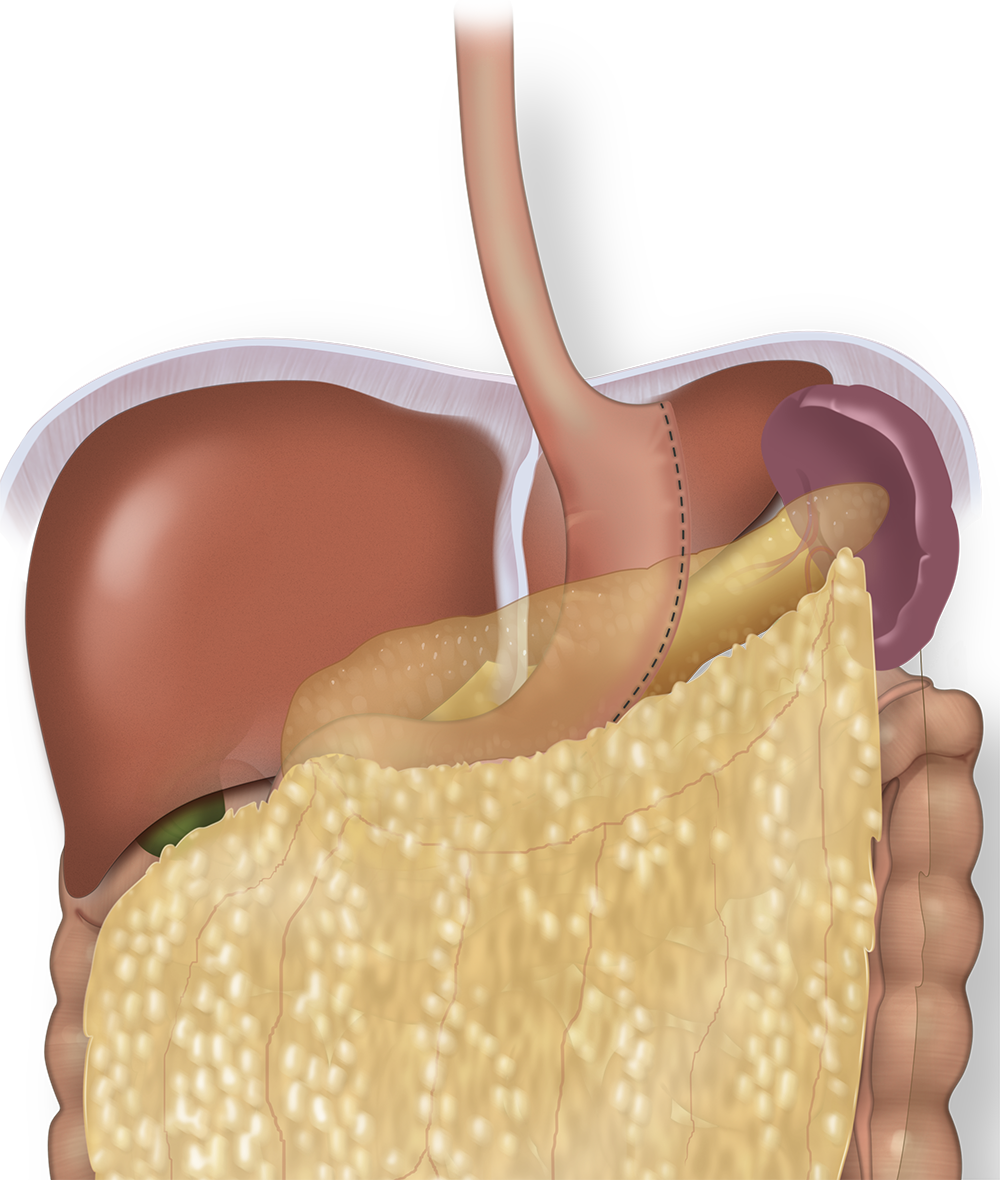
Laparoscopic sleeve gastrectomy (SG) also known as gastric sleeve surgery is a procedure in which a portion of the stomach is surgically removed with small cuts known as laparoscopic surgery. The procedure is performed on obese and morbidly obese patients to aid weight loss and resolve or improve overall health with respect to obesity related co-morbidities such as diabetes, sleep apnea, osteoarthritis, and hypertension. Sleeve gastrectomy has gained wide acceptance over the last ten years as an independent surgical procedure for treating obesity.
It is named a 'sleeve gastrectomy' because of the sleeve that is formed by surgically stapling the edges of the stomach. The stomach size can be reduced to as little as 15% of the original size. The small size is achieved by dividing the stomach on its vertical axis and preparing a small, long pouch. This procedure is typically performed laparoscopically and is a non-reversible procedure.. As a result of this reduction of stomach size, a person feels fuller upon eating a relatively small amount, body metabolism is altered and the craving for food is reduced.
What happens during laparoscopic sleeve gastrectomy?
Steps of the Sleeve
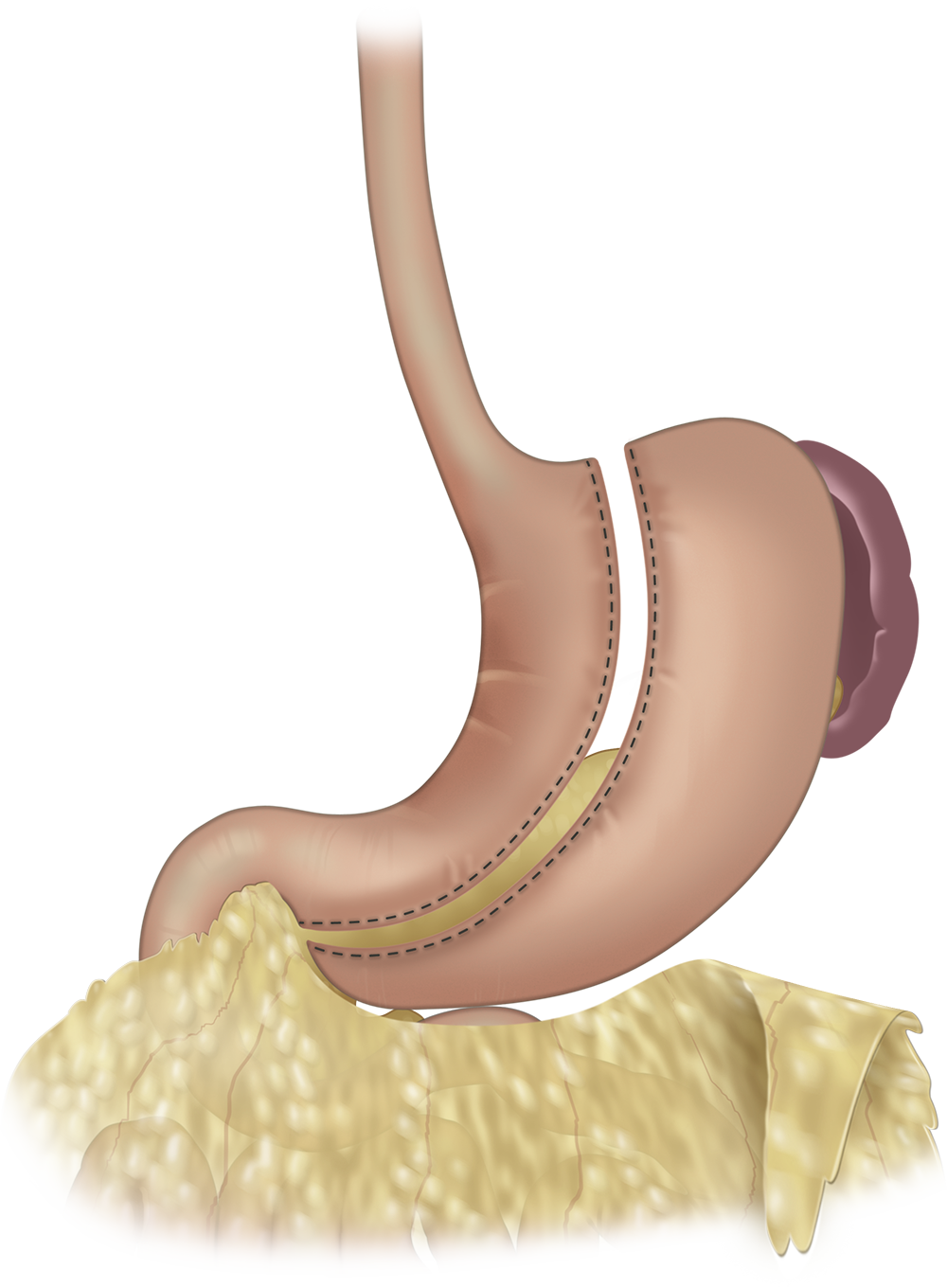
Laparoscopic sleeve gastrectomy is a restrictive procedure that reduces the size of the stomach but does not alter the path of the digestive system or the stomach pylorus. Because the route of ingested food through the gastrointestinal tract is not shortened nor altered, the absorption of nutrients is not significantly changed. A patient is hypothetically less dependent on vitamin supplements as the food is absorbed in the same more natural manner. Although the small intestine is not altered, the long-term effects of sleeve gastrectomy on nutrient absorption need to be better understood, as the size of the stomach can be reduced by as much as 85%.
The operative time of the sleeve gastectomy roughly varies between thirty minutes to two hours. On an average, patients stay in the hospital for one to three days. Similar to other bariatric procedures, return to normal activities and office work usually takes a fortnight. Your post-operative adherence to lifestyle regulations as presented by Dr. Belsley and your surgical team will play a large role in your ultimate success. You will be on a liquid and semi-liquid diet during the first few weeks after the surgery.
After the first month, there are few concrete food restrictions forced by the anatomical changes and a common sense approach and dedication to a life-long diet are necessary. Calorie rich foods and items that are difficult to digest will remain problematic. Smaller portion sizes are advised. You should chew the food properly to ensure that there is less bulk that reaches the digestive system. A calorie restrictive diet with a balance between the quantity and quality of food consumed along with regular exercise is the key to achieving and maintaining a healthy weight after surgery.
What are the differences of laparoscopic sleeve gastrectomy versus laparoscopic gastric bypass?
There are important differences in how the two operations affect the digestive system for their treatment of morbid obesity. During gastric bypass, the original stomach is left in place. Food travels from the pouch directly into the re-routed intestines. During the sleeve gastrectomy the stomachis removed. Food therefore travels along its original path. The fact that the food does not empty directly into the small intestine helps prevent dumping syndrome that sometimes occurs after gastric bypass.
The laparoscopic sleeve does not require any alteration of the small intestine. The sleeve may be preferable to a gastric bypass in patients who have had multiple surgical procedures in the past who are expected to have intestinal adhesions. The sleeve also is relatively far away from the colon and therefore the sleeve may be a preferred operation for those patients with a strong history of colon cancer who may eventually require a colon resection.
Intestinal Absorption
There are hypothetical benefits with hormonal changes responsible for satiety after laparoscopic sleeve gastrectomy. For example, a portion of the stomach that is removed produces a hormone called Ghrelin. This removal of the portion the stomach most responsible for producing Ghrelin is thought to play a role in causing a person to feel less hungry. Although not yet completely understood, with less stomach, there should be less of this hormone and therefore a decrease in the feeling of hunger.
Bariatric patients typically report that their subjective feeling of hunger is surprisingly reduced for the first few months after bariatric surgery. This reduced sensation of hunger is different for each patient but typically lasts sometime between one month and one year. This decreased sensation of hunger also correlates with the rapidity of weight-loss after the operation. Despite the fact that this Ghrelin producing portion of the stomach is permanently removed, feelings of hunger unfortunately return after approximately one year.
The procedure originated as a bridge or preliminary operation to biliopancreatic diversion surgery, however today is typically performed as a stand-alone definitive surgery. Laparoscopic sleeve gastrectomy represents an additional surgical option in high-risk patients who can't predictibably tolerate the technical rigors of a gastric bypass operation.
Results and research on the laparoscopic sleeve gastrectomy
Data gathering on the sleeve gastrectomy is an ongoing process. Present results from research on the effects of the procedure show that weight loss from sleeve gastectomy is less than what is achieved after gastric bypass. Data varies widely with regards to long-term follow up and some would suggest that the long-term weight loss is similar between both operations. Dr. Belsley has noticed over the years that the weight-loss achieved during a sleeve is not as long-lasting as that with the gastric bypass.
One side effect of the gastric sleeve is that esophageal acid-reflux likely worsens with time. Some degree of acid reflux in the morbidly obese is due to dietary choices as well as increased abdominal pressures and therefore improves after weight-loss surgery. The sleeve negatively affects the motility of the esophagus as well as how the stomach is able to empty acid and therefore acid reflux is a common complaint years after the sleeve has been performed. This acid reflux is usually minor and typically successfully treated with dietary changes and medications
Stomach Removal

Over the years, improved clinical outcomes in terms of weight loss and controlling comorbidities has resulted in greater acceptance for laparoscopic gastric sleeve surgery not only for the super-obese but also for obese patients with a lower BMI. The technical simplicity of the procedure, durable weight loss, and fewer post-operative restrictions on diet are reasons why laparoscopic sleeve gastrectomy is gaining scientific acceptance and now represents a popular surgical option to treat morbid obesity.